“The inevitable, but unpredictable, appearance of new infectious diseases has been recognized for millennia, well before the discovery of causative infectious agents. Today, however, despite extraordinary advances in development of countermeasures (diagnostics, therapeutics, and vaccines), the ease of world travel and increased global interdependence have added layers of complexity to containing these infectious diseases that affect not only the health, but the economic stability of societies.”
Source: Morens, David M, and Anthony S. Fauci, ‘Emerging Infectious Diseases: Threats to Human Health and Global Stability’, PLoS Pathogens, 9 (2013), e1003467 http://dx.doi.org/10.1371/journal.ppat.1003467 (open access)
*****************************
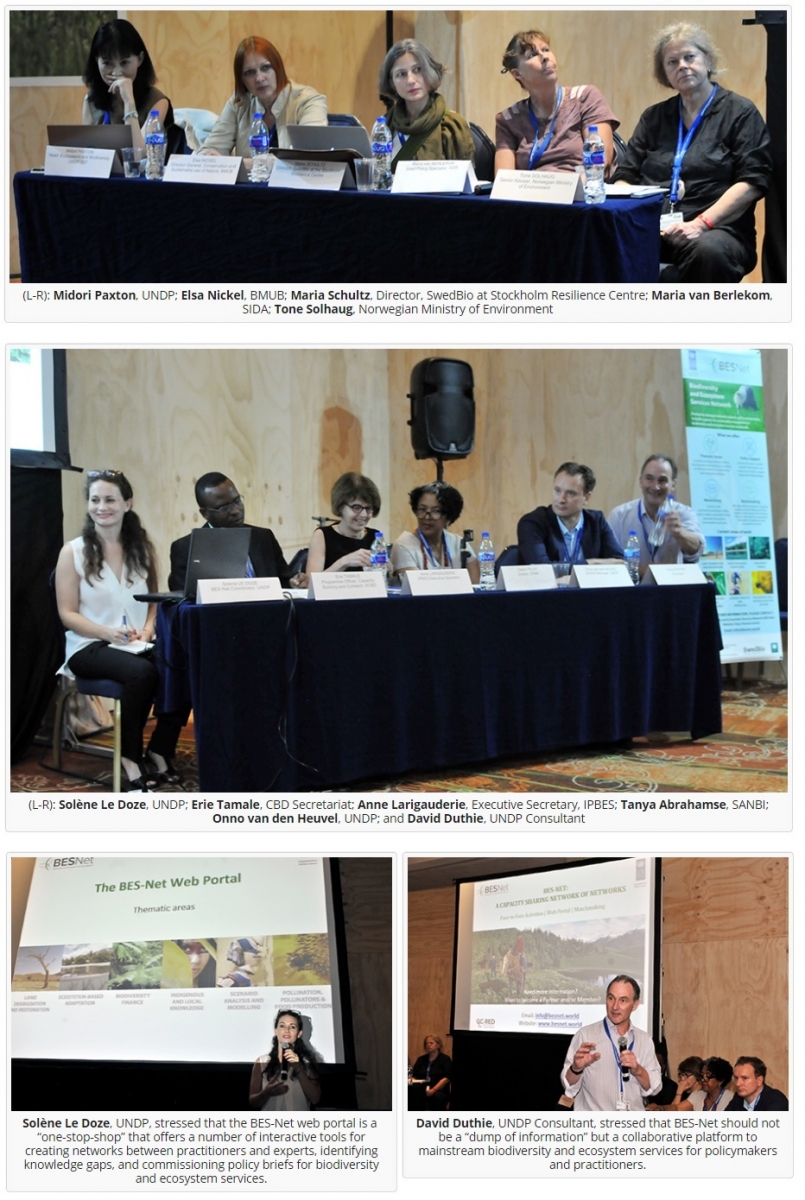
This BES-Net Op-Ed series #1 explores the origin of the COVID-19 pandemic and measures necessary to prevent the next pandemic. A few months ago, hardly anyone except a few dedicated scientists and medical researchers was paying much attention to coronaviruses. If you now type “coronavirus” into a well-known search engine, it finds over 2.5 billion results – never has so much research and writing (about a virus) been created in so short a space of time. Yet the virus still appears to have the upper hand.
Now, in June 2020, almost the entire global population of 7 billion persons has become aware of the SARS-COV-2 coronavirus, and its associated disease, COVID-19, including most likely, and tragically, some of the 103 indigenous groups in the Brazilian Amazon who have been trying to maintain “self-isolation” from modern civilization itself. Although no-one in the world was immune to the SARS-COV-2 virus when it spilled over in China late last year, indigenous communities, lacking historical exposure to a wide range of human diseases, living is closed intimate groups, and lacking adequate health systems, tend to fare worse in epidemics. In addition, the COVID-19 pandemic is unleashing a number of other threats to indigenous communities who play a key role in biodiversity conservation world-wide (see here and here).
The precise origins of this coronavirus are still not clear, except that it almost certainly spilled over from animal to human somewhere in China, probably late last year, leading to an initial outbreak in December 2019 linked to a wet food market in Wuhan, Hubei Province (1, 2). The rest, it could be said, is history.
|
The International Committee on Taxonomy of Viruses (ICTV) announced “severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)” as the name of the new virus on 11 February 2020. This name was chosen because the virus is genetically related to the coronavirus responsible for the SARS outbreak of 2003. While related, the two viruses are different.
The World Health Organization (WHO) announced “COVID-19” as the name of this new disease on 11 February 2020, following guidelines previously developed with the World Organisation for Animal Health (OIE) and the Food and Agriculture Organization of the United Nations (FAO). Source: WHO website – https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed 25th May 2020) |
SARS-CoV-2 virus most probably has its ecological reservoir in bats. All SARS-CoV-2 virus strains isolated from humans to date are closely related genetically to coronaviruses isolated from bat populations, specifically bats from the genus Rhinolophus, commonly known as horseshoe bats (3). Horseshoe bats may come into contact with humans because they are hunted for food in several regions of the world, particularly Sub-Saharan Africa, but also Southeast Asia, and some species, or their guano, are used in traditional medicine in Nepal, India, Vietnam, and Senegal (4).
Those scientists and medical researchers who study emerging infectious diseases (EIDs) have been warning governments that, as humans population grow in number, encroach further into wild habitat, intensify and industrialise our agriculture, especially with regard to livestock, move stuff and ourselves around the world further and faster, and neglect national and personal health, new emerging zoonotic diseases become statistically inevitable, whilst remaining, to some extent, geographically, and temporally unpredictable.
This work, and the epidemics that have already occurred (e.g. SARS, MERS, Ebola, Zika, etc.), has been admirably related in science journalist David Quammen’s 2012 book “Spillover: Animal Infections and the Next Human Pandemic” as well as his shorter article from the New York Times in 2013 on “Disease: The Next Big One”. In an interview to Orion Magazine in March 2020, Quammen responded to the question: “Why didn’t we see this [COVID-19] coming?” as follows:
“The warnings were there. The scientists who work on these things knew that coronaviruses should be high on the watch list, because coronaviruses mutate often and therefore evolve quickly. I was told ten years ago: ‘Beware of a new virus, maybe a coronavirus, emerging from a wild animal, maybe a bat’. Those were the warnings I put into Spillover.”
Scientists now estimate over 60% of around 1,500 known human infectious diseases are zoonotic and, of those classified as “emerging”, almost 50% are zoonoses (5, 6).
Clearly, it is impossible to monitor such a large number of potential risks, so scientists have been trying to find ways to prioritize those that pose the greatest risk. This can be done in a number of ways. First, one can ask which taxonomic groups of animals pose the greatest risk of spillover. Most scientists agree that three mammalian orders pose the greatest risk for spillover of zoonoses into humans – these are primates, rodents and bats – but each for different reasons (7).
We humans are, of course, primates ourselves, so taxonomic relationship, plus use of primates as bushmeat, explain most of the risk from this group (8). Rodents make up around 50% of all mammalian species and many live short, hyper-active lives, and have evolved to invest less in strong immune systems, making them more susceptible to diseases during their brief lives (9).
In 2015, researcher Angela Luis and colleagues asked the question: “A Comparison of Bats and Rodents as Reservoirs of Zoonotic Viruses: Are Bats Special?” and answered it in the affirmative (10). Bats are the only mammals which fly, which places a high metabolic demand on their bodies, with heartbeats rising to around 1000 beats per minute whilst flying. Physiological adaptation to this high stress has altered their immune systems in ways that make them tolerant, rather than resistant, to virus infections, allowing them to act as “efficient” ecological reservoirs for potential zoonoses (11). When coupled with their large home ranges and migrations, plus roosting in mixed species groups in caves or trees, some species of bats appear to have become a perfect “melting pot” for zoonoses, and coronaviruses especially appear, to have taken advantage of the “bat-pot”. It has been estimated that there could be over 3,000 different strains of coronavirus present in bats (12), and hundreds have already been identified (13).
So, if we know which are the high risk animals, then the places where these animals and human are most likely to meet become “pinch-points” where cost-effective surveillance and monitoring could occur. Using a global database of infectious zoonoses, researchers have developed probability maps of potential spillover, with Southeast Asia, South Asia and parts of Central and West Africa identified as major hotspots due to their high mammalian biodiversity in natural habitat (tropical forest), but also with high levels of land use change as a result of, for example, deforestation, agricultural expansion and mining (14).
These advances in our ecological knowledge of EIDs provide two clear messages:
- the probability of further emerging infectious diseases with pandemic is increasing and will continue to increase unless significant changes to our socio-economic systems are put in place. The same changes, especially in land use through natural habitat restoration, could also provide significant co-benefits for both biodiversity and climate change, as highlighted by senior IPBES coordinators in a recent guest article (15); and
- the increasing frequency and severity of emerging zoonoses means that an “adaptive” approach – responding to EIDs after they emerge – is no longer neither sufficient nor affordable, and that management plans, based on mitigation of risk, are now more cost-effective (16). For example, SARS cost an estimated US$30–50 billion despite causing illness in fewer than 9,000 people (17) and the ongoing costs of the COVID-19 pandemic are already estimated to be several trillions of dollars (18).
After we have managed to contain and control the current COVID-19 pandemic, how might we change our policies to mitigate future risk?
“One Health” is a term used when approaches to tackling disease (particularly zoonoses) consider all components that might lead to, or increase, the threat of disease. These include environmental and ecological/wildlife components, as well as domestic animal and human factors. The latter would encompass behavioural, as well as medical issues, including cultural, political and other socio-economic drivers that might result in disease occurrence or spread (19).
EID control strategies based on mitigation of risk rather than adaptation will vary depending on the particular threat and potential transmission pathways. Therefore, let’s turn the focus back on viruses, and coronaviruses in particular, and especially what can be done to reduce risk before, and in the early stages of, a disease spillover using a 4-step framework outlined in A of Figure 1 below (B is an expansion of A Step1 & 2 with added detail) (20).
Source: University College London (2016)
Step 1 – Pathogen in natural host
Rapid improvement in molecular biotechnology makes identification and monitoring of potential spillover zoonoses possible, given sufficient funding and effort. For example, in 2009, the USAID Emerging Pandemic Threats (EPT) PREDICT project became the first global-scale co-ordinated program designed to conduct viral discovery in wildlife reservoir hosts, and to characterize the ecological and socioeconomic factors that drive their risk of spillover. In 2018, the same researchers proposed a follow-on Global Virome Project (GVP) to document an estimated 600,000-800,000 viruses with spillover potential (not all to humans) (21). Clearly, monitoring almost a million viruses is not practical, so two additional criteria can used to narrow the search:
- focus research on wildlife species, like bats, that harbour a number of (related) viruses at the same time. For coronaviruses, this appears to be particularly important because the viruses evolve, not just by mutation, but also by recombination between virus strains within the same host. This appears to be exactly how the SARS-CoV-2 gained its ability to spillover into humans and spread between humans directly (22).
- focus monitoring on viruses that are found in a number of different species, especially those in close proximity to human populations (e.g. livestock and wild food animals), in addition to changing land use to provide greater separation between high risk habitats and local communities because this indicates a higher potential to “jump” across to other species (7).
Step 2 – Localized spillover for animal to humans
Even with all the measures above, there will be, and always have been, isolated spillover events into humans or our domesticated animals. Historically, the majority of these events would cause some localised disease and, depending on infectivity and virulence, would either die out naturally, or be controlled by local preventative measures. For example, a cholera outbreak in London in 1854 was controlled when a local doctor removed the handle from a contaminated water pump. Regular surveillance monitoring and better regulation of potential spillover hotspots, such as local communities living adjacent to high biodiversity forests, or bat roosts, hunters and sellers in the bushmeat and wildlife trade markets. Exactly, this kind of localised surveillance has been carried on coronaviruses in China as a proof of principle (23), but would need to be greatly scaled up to provide an effective barrier to spillover.
Step 3 – Propagation cycle – human to human spread
As we are seeing with the current COVID-19 pandemic, if a virus can spread from human to human directly, and especially if spread can occur before symptoms show, then a local spillover has the potential to rapidly spread and become an regional or global problem.
The unprecedented research effort being undertaken to gain control of the current pandemic will undoubtedly have secondary benefits in the form of organizational, product and process innovations to cope with future viral threats. This should include the expansion of hospital capacity and testing capabilities, reduction of diagnostic and health system delays, perhaps using artificial intelligence. In addition, new information and communication technologies for reducing and/or eliminating viral spread between infected and susceptible individuals need to be developed, plus speeding the development process for effective vaccines and antivirals that can counteract future global public health threats.
Source: UNEP & ILRI (2020)
The above Figure shows how a combination of the above three steps can dramatically reduce the severity and longevity of future spillover events, with corresponding social and economic benefits (24). In the Figure A, lack of these early actions leads to large outbreaks, either in domestic animals or humans, or both. In the Figure B, “forecasting readiness”, “early detection” and “control operations” correspond to the three steps described earlier, resulting in much less disease transmission to domestic animals and humans. Achieving “One Health” though better pandemic preparedness and rapid mitigation should be built into all national efforts to achieve the Sustainable Development Goals (25).
References
1. Tang, Xiaolu et al. (2020 ‘On the Origin and Continuing Evolution of SARS-CoV-2’, National Science Review, 395, 565 http://dx.doi.org/10.1093/nsr/nwaa036 (open access)
2. Zhou, Peng et al. (2020) , ‘A Pneumonia Outbreak Associated with a New Coronavirus of Probable Bat Origin’, Nature, 579, 270–73 http://dx.doi.org/10.1038/s41586-020-2012-7 (free access)
3. Li, Xiang et al. (2020) ‘Bat Origin of a New Human Coronavirus: There and Back Again’, Science China Life Sciences, 63, 461–62 http://dx.doi.org/10.1007/s11427-020-1645-7 (free access)
4. https://en.wikipedia.org/wiki/Horseshoe_bat (accessed 31st May 2020)
5. Taylor, Louise H, Sophia M Latham, and Mark E J Woolhouse (2001) ‘Risk Factors for Human Disease Emergence’, Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 356, 983–89 http://dx.doi.org/10.1098/rstb.2001.0888 (free access)
6. Karesh, William B. et al. (2012), ‘Ecology of Zoonoses: Natural and Unnatural Histories’, The Lancet, 380 (2012), 1936–45 http://dx.doi.org/10.1016/S0140-6736(12)61678-X (free access)
7. Olival, Kevin J. et al. (2017) Host and Viral Traits Predict Zoonotic Spillover From Mammals’, Nature, 546, 646–50. http://dx.doi.org/10.1038/nature22975
8. Locatelli, S. & Peeters, M. (2012) Non-Human Primates, Retroviruses, and Zoonotic Infection Risks in the Human Population. Nature Education Knowledge 3(10):62; https://www.nature.com/scitable/knowledge/library/non-human-primates-retroviruses-and-zoonotic-infection-59119998/ (free access)
9. Lee, K A, ‘Linking Immune Defenses and Life History at the Levels of the Individual and the Species’, Integrative and Comparative Biology, 46 (2006), 1000–1015 http://dx.doi.org/10.1093/icb/icl049 (free access)
10. Luis, Angela D. et al. (2013) ‘A Comparison of Bats and Rodents as Reservoirs of Zoonotic Viruses: Are Bats Special?’, Proceedings of the Royal Society B: Biological Sciences, 280 (2013), 20122753 http://dx.doi.org/10.1098/rspb.2012.2753 (free access)
11. Hayman, David T S, ‘Bat Tolerance to Viral Infections’, Nature Microbiology, 4 (2019), 728–29 http://dx.doi.org/10.1038/s41564-019-0430-9 (free access)
12. Anthony, Simon J. et al. (2019) ‘Global Patterns in Coronavirus Diversity’, Virus Evolution, 3 (2017), vex012 http://dx.doi.org/10.1093/ve/vex012 (open access)
13. Banerjee, Arinjay et al. (2019) ‘Bats and Coronaviruses’, Viruses, 11 (2019), 41 http://dx.doi.org/10.3390/v11010041 (open access)
14. Allen, Toph et al. (2017) ‘Global Hotspots and Correlates of Emerging Zoonotic Diseases’, Nat Commun, 8, 1–10 http://dx.doi.org/10.1038/s41467-017-00923-8 (open access)
15. Settele, Josef et al (2020) ‘COVID-19 Stimulus Measures Must Save Lives, Protect Livelihoods, and Safeguard Nature to Reduce the Risk of Future Pandemics’, Ipbes, 2020 https://ipbes.net/covid19stimulus [accessed 28 May 2020]
16. Pike, Jamison et al. (2104) Eonomic Optimization of a Global Strategy to Address the Pandemic Threat’, Proceedings of the National Academy of Sciences of the United States of America, 111 (2014), 18519–23 http://dx.doi.org/10.1073/pnas.1412661112 (free access)
17. https://www.who.int/whr/2007/media_centre/07_chap3_fig03_en.pdf (accessed 31st May 2020)
18. https://www.research.ox.ac.uk/Article/2020-04-07-the-economic-impact-of-covid-19 (accessed 1st June 2020)
19. Cunningham, Andrew A. et al. (2017) ‘One Health, Emerging Infectious Diseases and Wildlife: Two Decades of Progress?’, Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 372 (2017), 20160167 http://dx.doi.org/10.1098/rstb.2016.0167 (open access)
20. University London College (2016). ‘Map Shows Hotspots for Bat-human Virus Transmission Risks.’ Medical Express, https://bit.ly/2ZRekjt (open access).
21. Carroll, Dennis et al. (2018) ‘The Global Virome Project’, Science, 359 (2018), 872-74; http://dx.doi.org/10.1126/science.aap7463 (subscription required)
22. Li, Hongying et al. (2019) ‘Human-Animal Interactions and Bat Coronavirus Spillover Potential Among Rural Residents in Southern China’, Biosafety and Health, 1 (2019), 84–90 http://dx.doi.org/10.1016/j.bsheal.2019.10.004 (free access)
23. Li, Xiaojun et al. (2020) ‘Emergence of SARS-CoV-2 Through Recombination and Strong Purifying Selection’, Science Advances, eabb9153 http://dx.doi.org/10.1126/sciadv.abb9153 (free access)
24. United Nations Environment Programme and International Livestock Research Institute (2020). Preventing the Next Pandemic: Zoonotic diseases and how to break the chain of transmission. Nairobi, Kenya
25. Di Marco, Moreno et al. (2020) ‘Opinion: Sustainable Development Must Account for Pandemic Risk’, Proceedings of the National Academy of Sciences, 12, 202001655 http://dx.doi.org/10.1073/pnas.2001655117 (free access)